What is it?
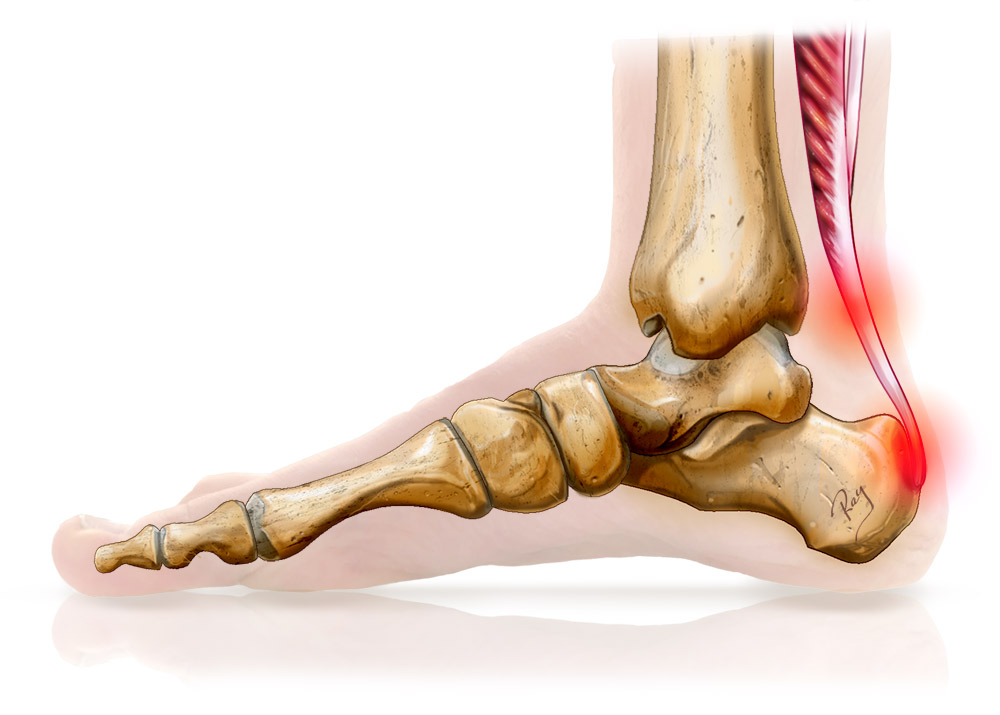
The Achilles tendon is the largest and most powerful tendon in the body. It is formed by the union of two muscles: the deep soleus muscle and the double superficial gastrocnemius muscle (or twins). These three muscles form the sural triceps. It is primarily responsible for the flexion of the ankle via its direct insertion in the calcaneus (the bones forming the heel).
The constraints on this tendon are extreme and can easily reach 8 to 10 times the body’s weight during certain physical activities such as running. Microtrauma is therefore inevitable and the viability of the tendon depends on the balance between these lesions and the body’s ability to heal.
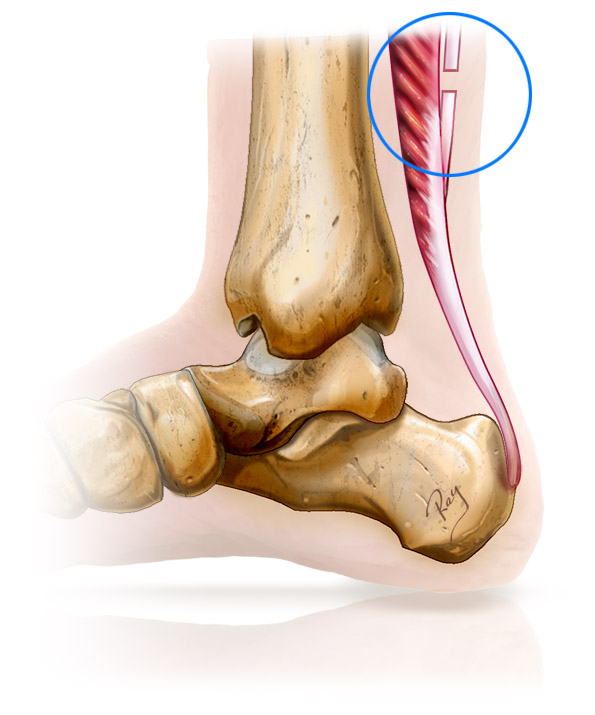
When tendon injuries occur at a faster rate than they heal, the Achilles tendon thickens and enters into a state of chronic suffering. For many years this was referred to as tendinitis of the Achilles tendon. However, this name was incorrect as it refers to chronic inflammation while in this case the condition is a chronic degenerative one. For this reason, the term tendinopathy will be used for greater accuracy.
This condition has many causes but the most common is injury due to overload (sport, physical occupations, etc.) and gastrocnemius equinus. Gastrocnemius equinus refers to the shortening of the tendon that is a tributary of the gastrocnemius muscle. This places major stresses on the Achilles tendon and forces the ankle into a flexion position. Gastrocnemius equinus is also responsible for very many foot and ankle disorders.
Depending on the location of the injury, these conditions are referred to as either non-insertional tendinopathy (located around 4-5 cm from the heel) or insertional tendinopathy (located at the insertion of the Achilles tendon on the heel). These two types of Achilles tendon injuries have different causes and require very different treatments and must be clearly distinguished. In particular, cases of non-insertional tendinopathy affect 9% of runners and alone are responsible for ending the careers of 5% of professional athletes.
This section will mainly describe non-insertional tendinopathy. For more information on insertional tendinopathy, follow this link.